Aep Are Used by Hospitals Review Agency for Admission Screening
- Enquiry
- Open Access
- Published:
Effect of inappropriate admissions on hospitalization performance in county hospitals: a cantankerous-sectional study in rural China
Price Effectiveness and Resource Allocation volume 17, Article number:eight (2019) Cite this article
Abstract
Background
Inappropriate admissions cause excessive utilization of health services compared with outpatient services. However, it is however unclear whether inappropriate admissions crusade excessive use of health services compared with appropriate admissions. This written report aims to clarify the differences in the hospitalization performances between accordingly admitted inpatients and inappropriately admitted inpatients.
Methods
A total of 2575 medical records were obtained later on cluster sampling in 3 counties. Access ceremoniousness was assessed by appropriateness evaluation protocol (AEP). The propensity score matching (PSM) was computed to friction match patients in treatment and control group with like characteristics, and to examine the differences in the utilization of hospitalization services between the two groups. The samples were matched in two major steps in this study. In the first step, total samples were matched to examine the differences in the utilization of infirmary services between the two groups using 15 individual covariates. In the second stride, PSM was computed to analyze the differences between the two groups in different affliction systems using xiv individual covariates.
Results
For the whole sample, the inappropriate group has lower expenditure of hospitalization (EOH) (difference = − 0.12, p = 0.003) and shorter length of stay (LOS) (difference = − 0.73, p = 0.016) than the appropriate group. For number of clinical inspection (NCI), it has no statistically meaning difference (departure = − 0.39, p = 0.082) betwixt the two groups. Among different illness systems, no significant differences were observed between the two groups among EOH, LOS and NCI, except that the EOH was lower in the inappropriate grouping than that in the appropriate grouping for surgical affliction (difference = − 0.169, p = 0.043).
Conclusion
Inappropriate admissions have generated excessive health service utilization compared with advisable admissions, especially for internal diseases. The departments in charge of medical services and hospital managers should pay high attention to the wellness service utilization of the inappropriately admitted inpatients. Relevant medical policies should be designed or optimized to increase the ceremoniousness in health care service commitment and precision in clinical pathway management.
Background
Excessive utilize of health services leads to waste of health resource and unreasonable increase in medical costs. Information technology is an consequence of widespread concern across the globe. Inappropriate admission is one of the nearly severe issues in the excessive utilise of health services [one]. Inappropriate admission refers to a condition that the utilization of hospitalization services is non conducted on the basis of clinical needs [ii], and physicians act as patients' agents and therefore tin influence the choice of patients to use hospitalization services compared to outpatient services. Therefore, patients tend to choose the hospitalization services according to the physicians' advice. Access ceremoniousness can exist assessed past appropriateness evaluation protocol (AEP), which is an objective, effective and reliable tool used to evaluate the appropriateness of the admissions on the ground of inpatient's medical records [3,4,5,6]. AEP criteria can exist divided into 2 parts: medical service intensity and disease severity.
Some studies have pointed out that compared with outpatient services, inappropriate admissions cause excessive use of wellness services, including human resources, beds, medicines and health care funds [7]. Nonetheless, information technology is not articulate whether inappropriate admissions crusade excessive use of health services compared with advisable admissions. Though previous studies accept indicated that patients with less severe diseases tend to have shorter length of stay (LOS) in hospital, and therefore, consume less health resources [viii, 9], this does not mean that the relatively minor amount of health resources are consumed by inappropriately admitted patients. The reasons are every bit follows.
Commencement of all, patients' actual utilization of hospitalization services will exist afflicted by policies that related to inpatient service delivery in the infirmary such as standardized inpatient service provision policy and clinical pathway direction and then on. No matter admission is appropriate or non, the patient will receive health intendance services in accordance with the standards of hospitalization service process. In other words, medical treatments, nursing and examination are strictly implemented in accordance with the clinical pathway course [10], where the timing of diagnosis and treatment measures is clarified, the clinical process is programmed, and the inspection, treatment and nursing that should be done every 24-hour interval are clearly specified. The patient would receive corresponding clinical biochemistry inspection, for instance blood exam, urine test [xi], and they would spend a standard flow in hospital, and receive the prescribed dosage. In this style, it may consequence in a condition that inappropriately admitted patients take the like utilization of hospital services compared to those who are admitted appropriately. 2d, the patient'due south condition is in constant change with uncertainty. The alter of the patient's condition will touch the subsequent series of wellness services [12]. For instance, the symptoms of the appropriately admitted inpatients may relieve rapidly later hospitalization and require less handling methods, and accordingly, the length of stay may exist shortened. Patients who are admitted inappropriately may get worse, when the utilization of medical services will be more intense. In this case, the length of stay may exist extended and the expenditure of hospitalization will increment. Thirdly, the utilization of health services is greatly influenced by md's behaviors. On the one hand, co-ordinate to the prospect theory proposed past Kahneman [13], most people are take chances-averse when facing gain and risk preference when facing loss. People are more sensitive to loss than to gain. As a result, people are often wary of taking risks in the face of gains. In other words, irrespective of the ceremoniousness of admission, doctors may tend to adopt the most conservative treatment methods when they are non sure of the state of affairs in the procedure of diagnosis and treatment. This leads patients to do more clinical inspections, extend length of stay for observation and and then on, all of which will increase the use of health services. On the other paw, physician's behaviors will also be affected by the infirmary internal management system and bacon system. This generates behaviors that induces consumption or reduces service, etc. Thus, the relationship betwixt the appropriateness of access and the utilization of health services is unclear, which calls for further exploration.
A study of Bianco A has revealed that doctors adopt a conservative management style due to their risk aversion, which led to inappropriate admission and inappropriate follow-up hospitalization services [14]. This increased the length of stay, resulting in unnecessary waste of resource. Information technology is more than mutual in surgery departments. Velasco's [15] written report illustrated that patients who were not properly admitted had iii times the length of hospital stay compared to those admitted appropriately. Eriksen [16] has measured the proportion of inappropriate admission of internal medicine and the toll, and the findings suggested that not accepting inappropriate admission did non bring the infirmary the same pct of cost reduction.
Although some studies have explored the relationship between admission appropriateness and hospitalization services utilization, these studies also have some limitations. First, some of studies were based on the comparison of an inpatient instance itself. These studies were the evaluation of ceremoniousness of admission and services utilization after hospitalization. They were not compared with other similar or contrary cases. 2nd, although length of stay and hospitalization expenses were studied in the evaluation of health services utilization, there were little detailed studies on the utilization of clinical inspection. 3rd, and most importantly, bereft consideration of the severity of disease made the comparison of service utilization lack of accuracy. The divergence in disease severity and the change of illness condition volition affect the utilization, and therefore, the operation of hospitalization services. Inappropriate admission and those with appropriate admission both accept patients with mild and serious severity. Whether there is a divergence in the utilization of services, and if then, what are the differences in the efficiency of hospitalization service are still unknown, and await further study. In add-on, matching patients with similar illness characteristics is of great practical significance for accurate evaluation of medical quality, utilization of wellness services and rational allocation of health resources.
Based on AEP, the ceremoniousness of admission is evaluated from two aspects of medical service intensity and disease severity. The admissions rated every bit "inappropriate" indicate that the patients take a balmy illness, and the required medical service intensity for them is non big. Thus, in theory, the consumption of health resources for inpatients admitted inappropriately is smaller than those admitted accordingly. Thus, this study hypothesized that inappropriate inpatients have shorter length of stay (LOS), fewer number of clinical inspection (NCI), and lower expenditure of hospitalization (EOH) than those who are admitted appropriately and with similar characteristics, and to verify information technology. The principal contribution of this study relative to other similar studies is the adoption of propensity score matching (PSM) methodology. The PSM was used to friction match patients in appropriate and inappropriate admissions with like characteristics, and to examine the differences in the utilization of hospitalization services among them. This would enrich more contribution relative to other methods.
This report is expected to provide reference for the policy makers when adjusting and improving relevant medical policies in order to promote the appropriateness of health resource utilization and control unreasonable increment in hospitalization expenses.
Methods
Data source
Three counties were selected as the sample counties (Dingyuan in Anhui province in central China; Huining in Gansu province, Yilong in Sichuan province in western Cathay). The reimbursement and payment levels of the new rural cooperative medical scheme (NRCMS) in the three counties are similar.
Cluster sampling method was applied in this study. The largest and most capable public comprehensive hospital in each county was selected every bit a sample hospital. Medical records were the objects of sampling. In the sampling calculation, co-ordinate to the existing research [2], the estimated inappropriate admission rate P is 16%, and the relative tolerance δ = 0.09, the absolute tolerance d = 0.09 *P = 1.44%, the significance level α = 0.05, and the i-sided standard normal deviation Zα = 1.96. The equation of sample size (N) was as follows:
$${\text{N}} = ({{\text{Z}}_{\upalpha}}/{\text{d}})^{2} \times {\text{P}} (one - {\text{P}}) = (1.96/one.44\%)^{ii} \times 16\% \times (ane-16\%)=2489.93$$
(1)
Considering the quality of medical records, 900 medical records in 2017 were selected from each hospital. Firstly, admissions of infirmary delivery records in obstetrics were excluded considering the pertinence of AEP. Then, corresponding quantity of medical records were selected from the remaining departments co-ordinate to the proportion of patients in the department accounted for the total quantity of patients in all departments. At last, a total of 2575 medical records were screened as samples afterward eliminating the records that accept likewise many missing values and serious logic errors (Fig. 1). At that place were no missing values in outcome variables in the final samples.
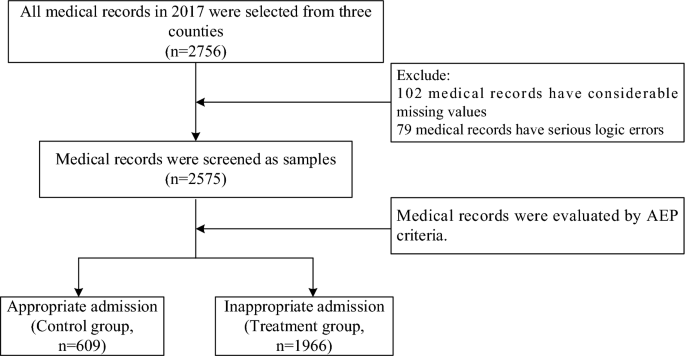
Study design and catamenia chart of the medical records selection and the allocate of those medical records in ii groups
All the medical records were evaluated by an adjusted AEP standard constructed in 2014 for canton hospitals in China [17] (Appendix). The records were evaluated past two trained judges respectively. The judges were members of the research team. A professional person training was held before they evaluating the admission ceremoniousness. Amid all the records, 609 admissions were regarded advisable (the control group) and 1966 were classified every bit inappropriate (the treatment group). This written report believes that in addition to the full general influencing factors (individual basic characteristics, external systems and policies, etc.) that impact the utilization of inpatient services, the constant development and modify of the disease itself is as well an important factor that cannot exist ignored. Based on the above considerations, this paper used a dynamic perspective to compare the utilization of wellness services after hospitalization in patients that with unlike admission appropriateness. This is also one of the highlights of this study. Based on such a enquiry perspective and the characteristics of the AEP criteria, the medical records were judged mainly co-ordinate to the patients' indications at the time of access (when some affliction indications may non exist fully manifested) rather than the final discharge results (when the disease indications are relatively comprehensive). Because disease indications are not fully manifested, it may be non easy to meet AEP'south criteria for "appropriate" admission. On this basis, it is possibly lead to overestimating the inappropriate access rate.
Study variables
Result variables
In this study, we utilize LOS, NCI and EOH as the outcome variables. These iii indicators can be used to describe the patients' utilization of services. LOS is a comprehensive alphabetize that directly measures hospital medical quality and management level [eighteen]. NCI is an important index to reflect services projects of inpatients receiving. EOH is a disquisitional alphabetize in the evaluation of wellness economics, which is the most direct reflection of health resource consumption [nineteen]. At the same time, considering that EOH may not conform to the normal distribution, the study logarithmically processed variable EOH and information technology conformed to the normal distribution later logarithmic transformation.
Explanatory variables
Since the selection of covariates by PSM was to include relevant variables that may affect the effect variables and processing variables every bit far as possible to satisfy the negligible hypothesis, this report included as many covariates equally possible in the medical records. There were 15 patient-level covariates in the written report, including gender, age, blazon of medical insurance, profession, marital condition, style of access, frequency of hospitalization, department in charge of handling, disease arrangement, having more than one disease, status of the patient upon admission, history of disease, with chronic diseases, health condition at ordinary times and receiving any surgery. Due to disease severity and considerations different, differences be in the utilization of health services among different age. Blazon of medical insurance too affects the utilization of wellness services. Especially with the development of NRCMS, the reimbursement ratio increases gradually, which promotes the release of patient medical service demand and increases the services projects [two]. The profession may touch the length of hospital stay. For instance, farmers may shorten the LOS regardless of the severity of the disease during busy seasons [20, 21]. Health condition at ordinary times, status of the patient upon admission, having more than one disease and affliction system are closely related to the changes of patients' weather condition later on hospitalization. These are variables that specially demand to exist paid attention to in this study. Changes in illness can affect LOS and utilization of services [22]. Whether receiving whatever surgery would influence their hospitalization results due to the take a chance of nosocomial infections and complications [23].
Propensity score matching (PSM)
In that location were differences in individual characteristics betwixt the treatment and command group, which will affect the comparison of the results of service utilization. Propensity scores were used to match each inpatient between two groups in similar conditions. PSM was used to balance observable covariates and reduce potential option bias [24, 25]. The samples were matched in two major steps in this study. In the commencement step, total samples were matched to examine the differences in the utilization of hospital services betwixt two groups using 15 individual covariates. In the 2nd stride, PSM was computed to analyze the differences in different illness systems, because the use of wellness services varies among disease systems. Disease system was divided into five groups (circulatory diseases, digestive diseases, respiratory diseases, surgical diseases and others). And then, inpatients in the handling and control group were matched in each group of disease. Xiv individual covariates were used except "disease arrangement". Therefore, it can be known whether there are pregnant differences in service utilization betwixt the ii groups in different diseases systems.
Statistical analysis
First of all, propensity score was obtained by incorporating the covariates into the logit model. So, kernel matching was used to match each patient in the handling group with like analogue patients in the control group (i-to-one matching) based on propensity score. The matching result of kernel method is good in terms of accuracy and it was summarized through literature in the field of health services [24, 26]. Finally, we calculated the boilerplate treatment effect on treated (ATT), which reflects the average change level of the effect variable after controlling the covariates.
Assume that each inpatient i has two potential outcomes, \(Y_{i1}\) (care for, inappropriate admission) and \(Y_{i0}\) (control, appropriate admission). The average effect of the treatment is given by \(E(Y_{i1} - Y_{i0} )\). Withal, as \(Y_{i0}\) and \(Y_{i1}\) cannot be observed simultaneously for the same inpatient, the ATT is calculated instead:
$$ATT = E(Y_{i1} |D_{i} = 1) - E(Y_{i0} |D_{i} = 1)$$
(2)
where \(D_{i}\) is the dichotomous indicator of handling, with 1 indicating that inpatients i are admitted inappropriately, and 0 are admitted appropriately. Stata 15.0 software (Stata Corp LP, College Station, TX, USA) was used for statistical analysis in a Windows environment. The two-sided statistical significance level was fix at 0.05.
Results
Bones characteristics of the sample
As shown in Table 1, the three effect variables were significantly different betwixt the two groups (p < 0.01), and the mean value and standard deviation of treatment group was lower than that of the command group. Covariates were likewise significantly different (p < 0.05), except for gender, marital status, and frequency of hospitalization variables.
The matching effect and results of the PSM of the total samples
As Table 2 shows, the covariates of the treatment group and the command group were well counterbalanced afterwards matching (p = 0.928, mean bias = 1.7, median bias = 1.3).
In Table 3, in the whole sample, the EOH of treatment group was lower than that of control group (difference = − 0.12, p = 0.003) after matching. The control grouping has longer LOS than the treatment grouping (divergence = − 0.73, p = 0.016). In that location was no statistically significant deviation in the NCI between the 2 groups (divergence = − 0.39, p = 0.082).
The matching effect and results of the PSM of the samples in disease systems
As Table 4 shows, in illness systems, the covariates of the treatment group and the control group were well balanced after matching except respiratory disease (p = 0.093, mean bias = 4.threescore, median bias = iv.7).
In EOH outcome variable, the treatment group was lower than that of control group in surgical disease (difference = − 0.169, p = 0.043). There was no significant deviation in other disease groups (p > 0.05). In LOS and NCI outcome variables, in that location was no pregnant departure in all disease systems between two groups (p > 0.05).
Word
Propensity score matching has been widely used in the field of health economics since the 1990s [27]. It eliminates the selective bias and the mixed bias by matching the individuals in the treatment group with the appropriate comparable objects in the control grouping [28]. In this study, the resource consumption between advisable access and inappropriate access groups was compared past controlling the factors influencing the utilization of services. This method balances the problems caused by incomplete and inaccurate pairings [29]. Meanwhile, the results of multiple covariates acting together can exist expressed [30]. This makes the results authentic and comparable.
For the whole sample, with the similar basic characteristics, the patients admitted inappropriately had shorter LOS and lower EOH than those admitted appropriately. As a whole, the study indicates that the health service utilization of patients admitted inappropriately was less than that of patients admitted appropriately. This is basically in line with expectations. No departure in NCI was observed betwixt them. This indicates that inappropriate admission may result in overuse of clinical inspection services. In dissimilar affliction groups, in that location were some specific differences. Diseases were classified into internal and surgical diseases. Amongst surgical diseases, the EOH of inappropriate admission group was less than the appropriate admission group. As long every bit the patient needs surgery, he/she is piece of cake to accord with the AEP (A1, A4,) and be evaluated as an appropriate access. The cost of surgery, drug exchange and infusion, etc., will brand the EOH of the appropriate admission higher than that of the inappropriate admission. Thus, in terms of surgical diseases, inpatients admitted inappropriately will non swallow more wellness resources than those admitted appropriately.
The circulatory diseases, digestive diseases and respiratory diseases are internal diseases. There was no statistically pregnant difference in internal affliction in the EOH, LOS and NCI between the two groups. This is different from the comparison results of the surgical diseases. At that place are two possible explanations.
First, every bit organic disease, the cause of the internal diseases is circuitous and difficult to be identified and diagnosed [31]. It has hidden features, and the features of the disease may gradually become apparent after access. In this case, the means of diagnosis and treatment may increase after hospitalization among the inappropriately admitted patients. Second, the symptoms of patients admitted inappropriately did non change after access, just the consumption of resource was as much every bit that of patients admitted accordingly, which indirectly indicates that in that location exists avoidable consumption of health resources. It may be related to the salary system of public hospitals in Cathay. For years, under the status of market economy [32], doctors in public hospitals have been required to earn their own salary through business income. At the same time, the pricing of technical services is seriously low, and the human uppercase value of doctors is not fully reflected. The inappropriate salary structure and distribution factors has led to further distortion of incentive machinery [33]. Most obviously, "subsidizing medical services with medicine" has distorted the behaviors of medical staff, making them prescribe "big prescriptions" to pursue the maximization of economic benefits to protect their vital interests. They prefer to use expensive drugs, let patients do more than clinical inspections and extend the LOS of patients, resulting in increased hospitalization expenditures [34, 35]. Meanwhile, intense doctor–patient relationship at present has led to a condition that some medical staff conduct unnecessary clinical inspections and treatments on patients in order to avoid risks [36]. Besides, it is related to doctors' ain handling habits and lack of grasp of illness severity [37]. It is possible that after the patient admitted to hospital, doctors provide the services that they are accepted to, or treat patients according to the specified clinical pathways. Due to the lack of judgment on the severity of the disease, some services are unnecessary, peculiarly for patients who are not appropriately admitted to the hospital.
To solve these issues, it is necessary to reform the salary distribution system of public hospitals [38]. Public hospitals should meliorate the incentive mechanism of internal resource allotment by making doctors earnings more on the value of their labor than the quantity of their services. The combination of constructive motivation and supervision to the hospitals tin can promote the hospitals to improve efficiency, reduce service cost, shorten the LOS and reduce the induced expenditure. In improver, optimizing the clinical pathway management is necessary. The clinical pathway aims to optimize the service process, reduce the delay in illness treatment and waste product of resources, and provide patients with efficient and high-quality medical and nursing services [39]. Even so, it does not indicate that there is no overconsumption of resources. Studies have shown that the issue of reducing hospital costs through clinical pathway direction is limited [40, 41]. Clinical pathways can ameliorate the treatment effectiveness, just it does non reduce the length of stay or hospital costs [42]. Therefore, when implementing clinical pathway, it is necessary to consider the same disease with different severity and make clinical pathway more elaborate.
Limitations
This report has 4 limitations. At first, although PSM eliminates the selective bias and the mixed bias by matching the individuals, which makes the two groups more comparable, it merely controls the influence of measurable variables, and "hidden bias" may yet occur if option on unobservable variables exists. Second, the content of covariate indicators is express and cannot fully reflect the real situation of patients. Third, the medical records may not be authentic plenty, which may touch on the appropriateness evaluation. Finally, in the PSM process, kernel matching was selected to used. Although this method has skilful applicability in practice, in that location may exist other more suitable matching methods.
Conclusions
Inappropriate admissions accept generated excessive health service utilization compared with advisable admissions, especially for internal diseases. On the one manus, the NCI of inappropriately admitted inpatients had no significant deviation compared with appropriately admitted inpatients on the whole. On the other hand, when information technology comes to the disease systems, no significant differences existed betwixt the 2 groups among EOH, LOS and NCI, except that the EOH was lower amid the inappropriate group than the advisable grouping in surgical affliction. Policy makers need to pay more than attention to the utilization of wellness resources of inappropriately admitted inpatients. Relevant medical policies should be optimized to promote medical service providers' ceremoniousness of wellness service provision, and the clinical pathway management should be more than precise. At the same fourth dimension, patients should be guided to utilize health services appropriately.
Abbreviations
- AEP:
-
appropriateness evaluation protocol
- PSM:
-
propensity score matching
- EOH:
-
expenditure of hospitalization
- LOS:
-
length of stay
- NCI:
-
number of clinical inspection
- NRCMS:
-
new rural cooperative medical scheme
References
-
Nekoei MM, Amiresmaili M, Goudarzi R, et al. Investigating the appropriateness of admission and hospitalization at a education hospital: a case of a developing country. Iran J Public Health. 2017;46(12):1720–5.
-
Zhang Y, Zhang L, Li H, et al. Determinants of inappropriate admissions in county hospitals in rural China: a cross-sectional study. Int J Environ Res Public Health. 2018;15(6):1050.
-
Strumwasser I, Paranjpe NV, Ronis DL, et al. Reliability and validity of utilization review criteria: appropriateness evaluation protocol, standardized medreview musical instrument, and intensity–severity–discharge criteria. Med Intendance. 1990;28(2):95.
-
Vieira NB, Rodrã-Guez-Vera J, Ferrão E, et al. Appropriateness of hospitalization in a ward of internal medicine-using the appropriateness evaluation protocol. Acta Med Port. 2006;19(i):67–lxx.
-
Manckoundia P, Menu D, Turcu A, et al. Analysis of inappropriate admissions of residents of medicalized nursing homes to emergency departments: a prospective multicenter study in burgundy. J Am Med Dir Assoc. 2016;1:1. https://doi.org/10.1016/j.jamda.2016.04.017.
-
Brabrand G, Knudsen T, Hallas J. The characteristics and prognosis of patients fulfilling the appropriateness evaluation protocol in a medical access unit; a prospective observational study. BMC Health Serv Res. 2011;11(ane):152. https://doi.org/10.1186/1472-6963-xi-152.
-
Hammond CL, Pinnington LL, Phillips MF. A qualitative examination of inappropriate hospital admissions and lengths of stay. BMC Health Serv Res. 2009;9(one):44.
-
Rosenthal GE, Sirio CA, Shepardson LB, et al. Use of intensive care units for patients with depression severity of affliction. Arch Intern Med. 1998;158(ten):1144.
-
Manzoli L, Romano F, Schioppa FS, et al. On the use of disease staging for clinical direction: assay of untimely admissions in the Abruzzo Region, Italy. Epidemiol Biostat Public Health. 2004. https://doi.org/x.2427/6017.
-
Rotter T, Kinsman L, James EL, et al. Clinical pathways: effects on professional practise, patient outcomes, length of stay and hospital costs. Int J Evid Based Healthc. 2011;9(2):191–2.
-
Chen West, Ji G, Pu F, et al. The analysis of clinical pathway on impacting hospitalization days and expense of v types of diseases. Chin Med Rec. 2013;14(7):23–5. https://doi.org/10.3969/j.issn.1672-2566.2013.07.012
-
Berth BM, Ludke RL, Wakefield DS, et al. Human relationship between inappropriate admissions and days of care: implications for utilization direction. Hosp Health Serv Adm. 1991;36(3):421.
-
Kai D. Prospect theory: an assay of decision under take a chance. Econometrica. 1979;47(2):263–91.
-
Bianco A, Pileggi C, Rizza P, et al. An cess of inappropriate hospital bed utilization by elderly patients in southern Italy. Aging Clin Exp Res. 2006;18(three):249–56.
-
Velasco DL, García RS, de la Oterino FD, et al. Impact on infirmary days of care due to unnecessary emergency admissions. Rev Esp Salud Pública. 2005;79(5):541.
-
Eriksen BO, Kristiansen IS, Nord Eastward, et al. The cost of inappropriate admissions: a study of health benefits and resource utilization in a department of internal medicine. J Intern Med. 2010;246(4):379–87.
-
Zhang Y, Chen Y, Zhang Ten, et al. Current level and determinants of inappropriate admissions to township hospitals under the new rural cooperative medical system in China: a cross-sectional study. BMC Wellness Serv Res. 2014;fourteen(i):649.
-
Yang T, Shi Y. Talk over on definition and standard of average length of stay. Mentum Health Qual Manag. 2009;16(4):xiv–6. https://doi.org/10.3969/j.issn.1006-7515.2009.04.005.
-
de la Oterino FD, Ridao Chiliad, Peiró S, et al. Hospital at home and conventional hospitalization. An economic evaluation. Med Clín. 1997;109(vi):207–11.
-
Bingsheng KE. Low income of chinese farmers: what are the root causes? Trouble of Agric Econ. 2005;26(1):25–thirty. https://doi.org/10.3969/j.issn.g-6389.2005.01.006.
-
Funing Z, Jun H. To generate more off-farm chore opportunities as the key to increase the farmers' income. Issues Agric Econ. 2007. https://doi.org/10.3969/j.issn.k-6389.2007.01.014.
-
Lee HC, Chang KC, Lan CF, et al. Factors associated with prolonged hospital stay for acute stroke in Taiwan. Acta Neurol Taiwanica. 2008;17(ane):17–25.
-
Faulborn J, Conway BP, Machemer R. Surgical complications of pars plana vitreous surgery. Ophthalmology. 1978;85(2):116–25.
-
Dehejia RH, Wahba South. Propensity score-matching methods for nonexperimental causal studies. Rev Econ Stat. 1998;84(one):151–61.
-
Caliendo M, Kopeinig S. Some practical guidance for the implementation of propensity score matching. J Econ Surv. 2010;22(1):31–72.
-
Austin PC. Propensity-score matching in the cardiovascular surgery literature from 2004 to 2006: a systematic review and suggestions for improvement. J Thorac Cardiovasc Surg. 2007;134(v):1128–1135.e3.
-
Yanling L, Liqing Fifty. The study on health resource utilization performance of the new rural cooperative medical scheme: based on the empirical analysis of propensity score matching (PSM)'due south. Issues Agric Econ. 2009;(10):51–eight.
-
Bai H. A comparison of propensity score matching methods for reducing option bias. Int J Res Method Educ. 2011;34(1):81–107.
-
Baser O. Too much ado near propensity score models? Comparing methods of propensity score matching. Value Health. 2010;9(vi):377–85.
-
Pan West, Bai H. Propensity score interval matching: using bootstrap confidence intervals for accommodating estimation errors of propensity scores. BMC Med Res Methodol. 2015;xv(one):ane–nine.
-
Kunitz SC. The upshot of finasteride on the risk of astute urinary retention and the demand for surgical treatment among men with benign prostatic hyperplasia. J Urol. 1998;160(1):557–63.
-
Pan J, Qin Ten, Hsieh CR. Is the pro-competition policy an effective solution for China's public infirmary reform? Health Econ Policy Law. 2016;11(4):337–57.
-
Fu H, Li L, Li K, et al. An evaluation of systemic reforms of public hospitals: the Sanming model in China. Health Policy Plan. 2017;32(8):1135.
-
Zhang H, Hu H, Wu C, et al. Impact of China's public hospital reform on healthcare expenditures and utilization: a instance study in ZJ Province. PLoS I. 2015;10(11):e0143130.
-
Zhang Y, Ma Q, Chen Y, et al. Effects of public infirmary reform on inpatient expenditures in rural China. Wellness Econ. 2016;26:421–30.
-
Wei-Ping LI, Er-Dan H. Two key points of public hospital reform: public welfare and incentive mechanism. Wellness Econ Res. 2009;5:5–seven. https://doi.org/ten.3969/j.issn.1004-7778.2009.05.002.
-
Weiping L. Five measures for public hospital reform in China. Chin Health Econ. 2010;29(3):5–8. https://doi.org/10.3969/j.issn.1003-0743.2010.03.002.
-
Christensen T. Performance direction and public sector reform: the Norwegian Hospital Reform. Int Public Manag J. 2006;9(2):113–39.
-
Yingmei D, Chunling L, Lihong W, et al. Analyze the implement results of single disease clinical pathway in department of neurology. Chin Med Rec. 2011;12(11):25, 44. https://doi.org/10.3969/j.issn.1672-2566.2011.11.015.
-
Rotter T, Kinsman 50, James Eastward, et al. The furnishings of clinical pathways on professional person practice, patient outcomes, length of stay, and hospital costs: cochrane systematic review and meta-analysis. Eval Health Prof. 2012;35(1):3.
-
Deguang QI. Application of clinical pathway in quality management of hospital services. Chin Hosp. 2002;22(10):11–2. https://doi.org/x.3969/j.issn.1001-5329.2002.10.006.
-
Guangfeng YE, Hong Y, Pusheng Z, et al. Result evaluation of clinical pathway for chronic sinusitis. Chin Hosp. 2013;three:19–20. https://doi.org/x.3969/j.issn.1671-0592.2013.03.010.
Authors' contributions
JJC, YCC and HXG contributed to the conception and design of the project; JJC and YZ contributed to the analysis and interpretation of the data; HML, DS, XMH, DJ, SHL, MT and ZFC contributed to the data conquering and provided statistical assay support; JJC drafted the commodity. All authors supplied critical revisions to the manuscript and gave final approving of the version to be published. All authors read and canonical the final manuscript.
Acknowledgements
The authors thank the county hospitals of Dingyuan in Anhui province, Huining in Gansu province and Yilong in Sichuan province, for their willingness to provide us the information.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets used and/or analyzed during the current report are available from the respective author on reasonable request. Contact data: chenyingchunhust@163.com.
Consent for publication
Not applicable.
Ideals blessing and consent to participate
The information used in this report was obtained from the hospitals with their permission, and all information related to inpatients privacy was not extracted. The enquiry methods and investigation tools in this study were approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Engineering science (IORG No: IORG0003571).
Funding
This piece of work was supported by the National Natural Science Foundation of Mainland china (No. 71473096; No. 71673101). The funders had no role in written report blueprint, data drove and analysis, decision to publish or grooming of the manuscript.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Affiliations
Corresponding author
Appendix
Appendix
Meet Table v.
Rights and permissions
Open Access This article is distributed nether the terms of the Creative Eatables Attribution 4.0 International License (http://creativecommons.org/licenses/by/four.0/), which permits unrestricted utilize, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(due south) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Eatables Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zilch/1.0/) applies to the data made available in this article, unless otherwise stated.
Reprints and Permissions
About this article
Cite this article
Chang, Jj., Chen, Yc., Gao, Hx. et al. Issue of inappropriate admissions on hospitalization functioning in county hospitals: a cross-exclusive report in rural Cathay. Cost Eff Resour Alloc 17, 8 (2019). https://doi.org/10.1186/s12962-019-0176-v
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s12962-019-0176-5
Keywords
- Excessive utilization of health services
- Inappropriate admissions
- Propensity score matching
- Appropriateness evaluation protocol
Source: https://resource-allocation.biomedcentral.com/articles/10.1186/s12962-019-0176-5
0 Response to "Aep Are Used by Hospitals Review Agency for Admission Screening"
Postar um comentário