Easy to Remember Asthma Fnp Study Guide
The cardiovascular system is so vital that its activity defines the presence of life. The cardiovascular system begins its activity when the fetus is barely a month old and is the last body system to cease activity at the end of life.
More than 80 million Americans have one or more types of cardiovascular disease which include hypertension, coronary artery disease, heart failure, and other congenital cardiovascular defects. Because of the prevalence of cardiovascular diseases, nurses practicing in any setting should have a clear understanding of various conditions affecting the cardiovascular care.
To help you grasp the core concepts of Cardiovascular Care Nursing (or Cardiac Care Nursing), here are our visual nursing mnemonics and tips!
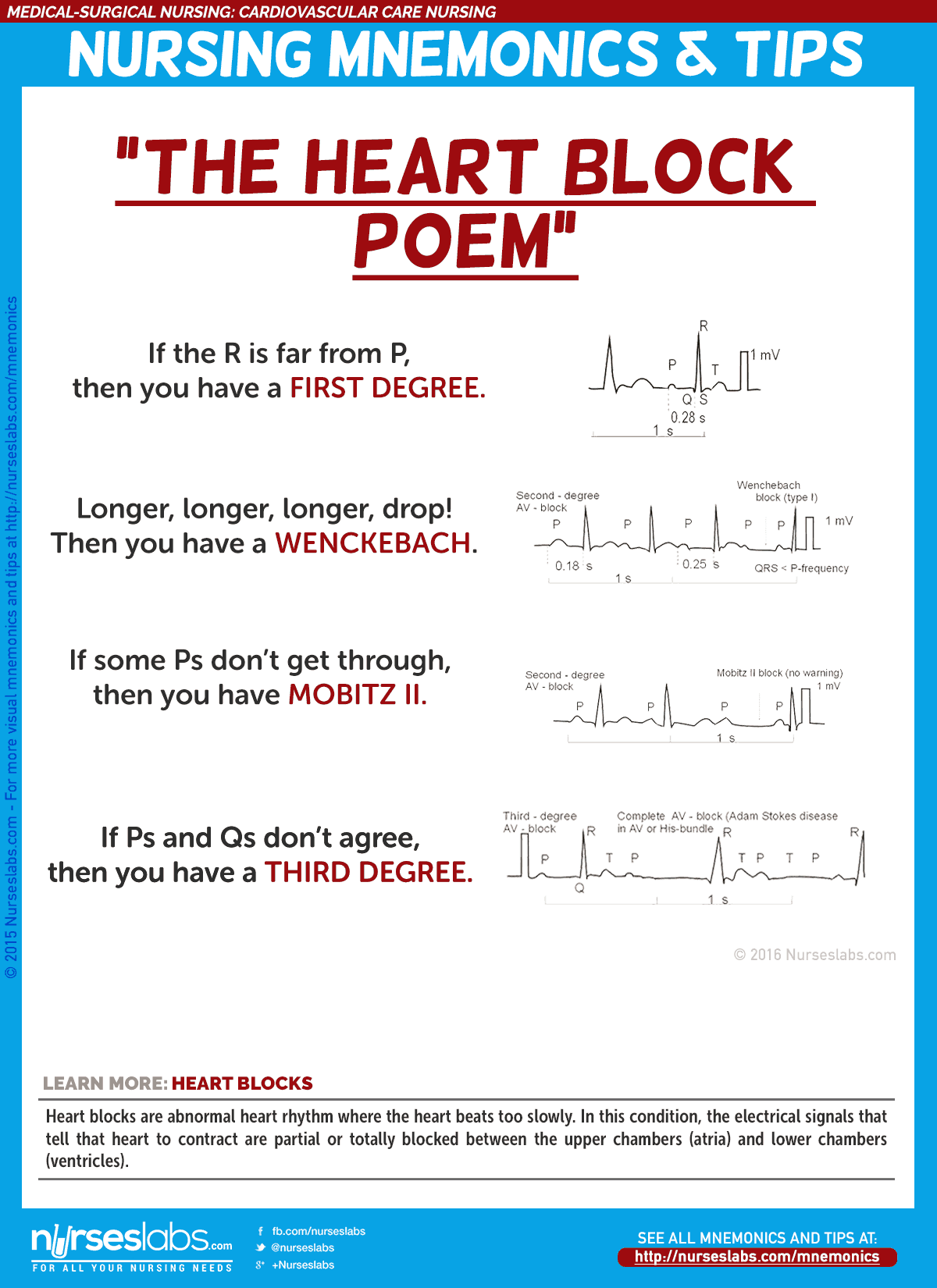
1. Heart Blocks: "The Heart Block Poem"
Heart blocks are abnormal heart rhythm where the heart beats too slowly. In this condition, the electrical signals that tell that heart to contract are partially or totally blocked between the upper chambers (atria) and lower chambers (ventricles).
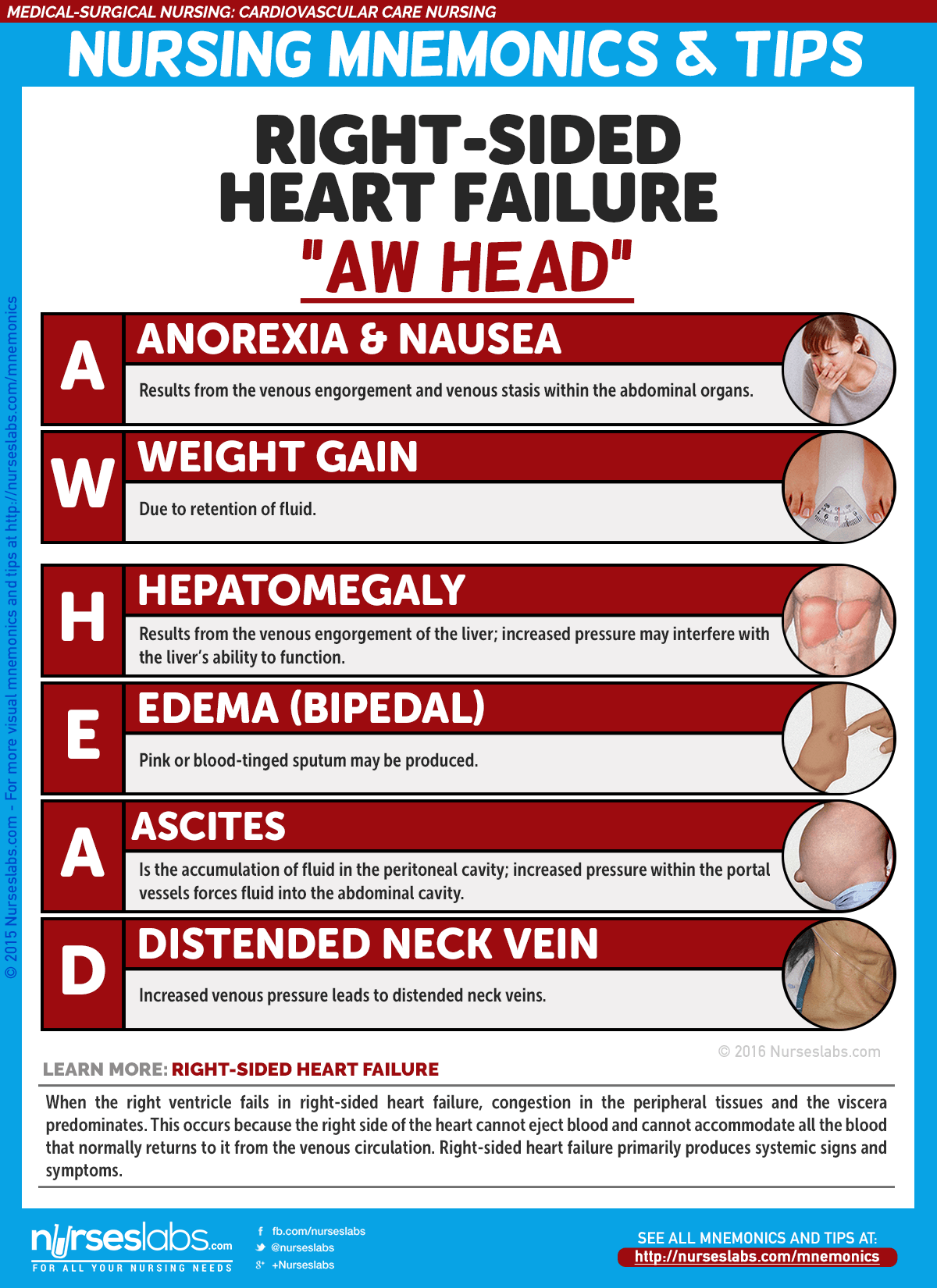
2. Right-Sided Heart Failure Manifestations: "AW HEAD"
When the right ventricle fails in right-sided heart failure, congestion in the peripheral tissues and the viscera predominates. This occurs because the right side of the heart cannot eject blood and cannot accommodate all the blood that normally returns to it from the venous circulation. Right-sided heart failure primarily produces systemic signs and symptoms.
- A: Anorexia and nausea
Results from the venous engorgement and venous stasis within the abdominal organs. - W: Weight gain
Due to retention of fluid. - H: Hepatomegaly
Results from the venous engorgement of the liver; increased pressure may interfere with the liver's ability to function. - E: Edema (Bipedal)
Edema usually affects the feet and ankles and worsens when the patient stands or sits for a long period. - A: Ascites
Is the accumulation of fluid in the peritoneal cavity; increased pressure within the portal vessels forces fluid into the abdominal cavity. - D: Distended neck vein
Increased venous pressure leads to distended neck veins.
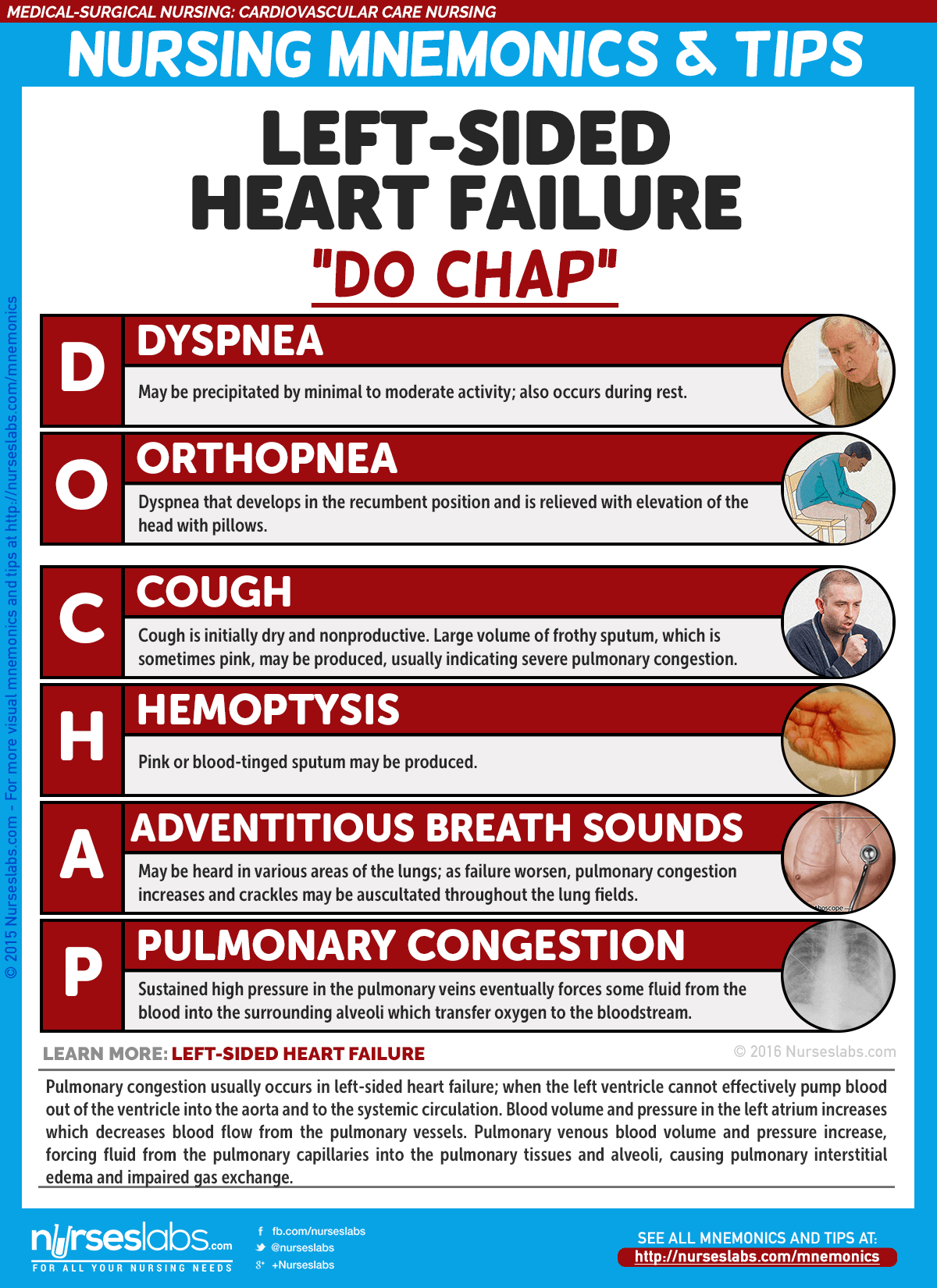
3. Left-Sided Heart Failure: "DO CHAP"
Pulmonary congestion usually occurs in left-sided heart failure; when the left ventricle cannot effectively pump blood out of the ventricle into the aorta and to the systemic circulation. Blood volume and pressure in the left atrium increases which decreases blood flow from the pulmonary vessels. Pulmonary venous blood volume and pressure increase, forcing fluid from the pulmonary capillaries into the pulmonary tissues and alveoli, causing pulmonary interstitial edema and impaired gas exchange.
- D: Dyspnea
May be precipitated by minimal to moderate activity; also occurs during rest. - O: Orthopnea
Dyspnea that develops in the recumbent position and is relieved with elevation of the head with pillows. - C: Cough
Cough is initially dry and nonproductive. Large volume of frothy sputum, which is sometimes pink, may be produced, usually indicating severe pulmonary congestion. - H: Hemoptysis
Pink or blood-tinged sputum may be produced. - A: Adventitious breath sounds
May be heard in various areas of the lungs; as failure worsen, pulmonary congestion increases and crackles may be auscultated throughout the lung fields. - P: Pulmonary congestion (crackles/rales)
Sustained high pressure in the pulmonary veins eventually forces some fluid from the blood into the surrounding microscopic air sacs (alveoli), which transfer oxygen to the bloodstream.
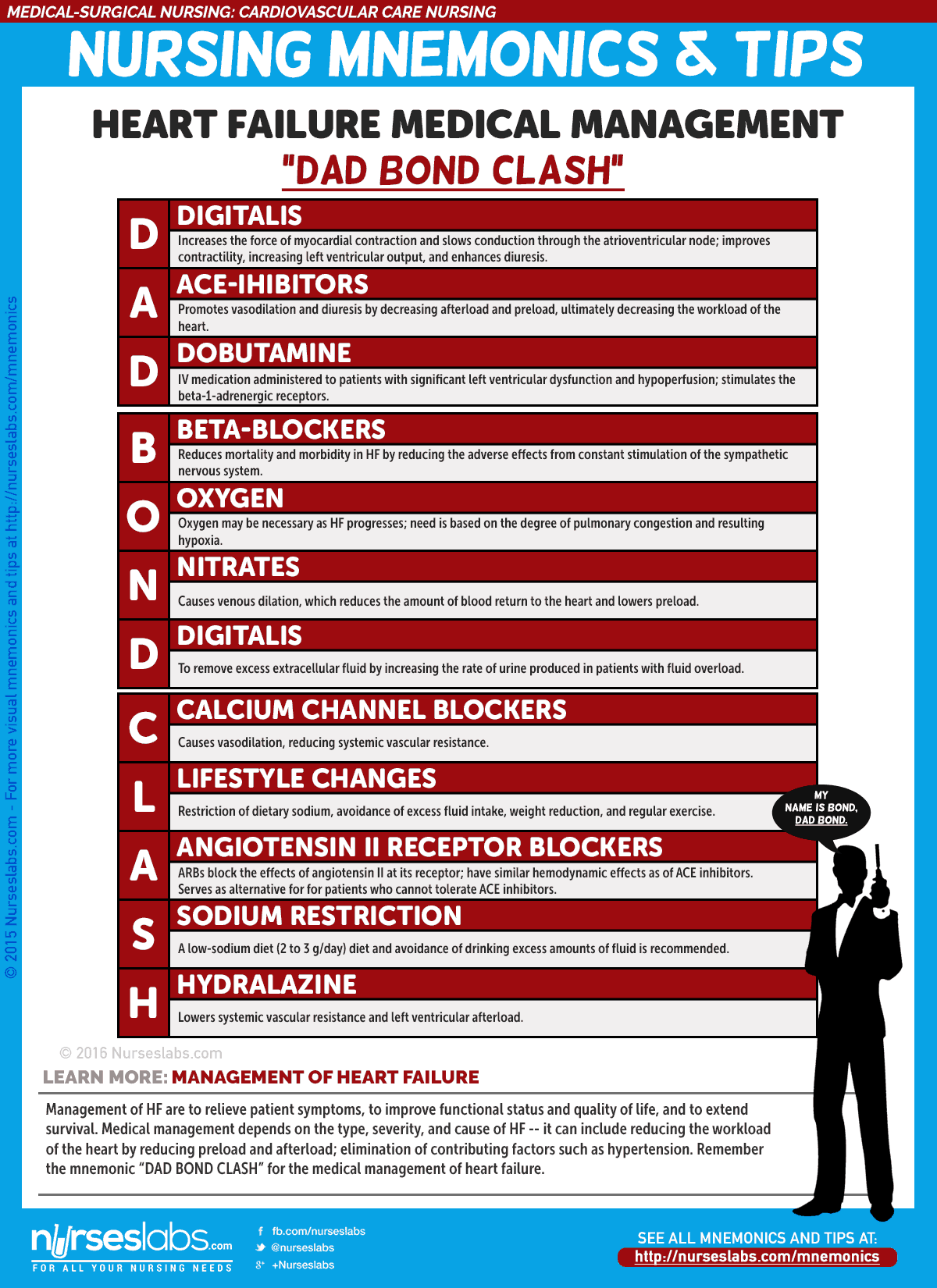
4. Management of Heart Failure: "DAD BOND CLASH"
Management of HF are to relieve patient symptoms, to improve functional status and quality of life, and to extend survival. Medical management depends on the type, severity, and cause of HF — it can include reducing the workload of the heart by reducing preload and afterload; elimination of contributing factors such as hypertension. Remember the mnemonic "DAD BOND CLASH" for the medical management of heart failure.
- D: Digitalis
Increases the force of myocardial contraction and slows conduction through the atrioventricular node; improves contractility, increasing left ventricular output, and enhances diuresis. - A: ACE Inhibitors
Promotes vasodilation and diuresis by decreasing afterload and preload, ultimately decreasing the workload of the heart. - D: Dobutamine
IV medication administered to patients with significant left ventricular dysfunction and hypoperfusion; stimulates the beta-1-adrenergic receptors. - B: Beta-blockers
Reduces mortality and morbidity in HF by reducing the adverse effects from constant stimulation of the sympathetic nervous system. - O: Oxygen
Oxygen may be necessary as HF progresses; need is based on the degree of pulmonary congestion and resulting hypoxia. - N: Nitrates
Causes venous dilation, which reduces the amount of blood return to the heart and lowers preload. - D: Diuretics
To remove excess extracellular fluid by increasing the rate of urine produced in patients with fluid overload. - C: Calcium Channel Blockers
Causes vasodilation, reducing systemic vascular resistance. - L: Lifestyle Changes
Restriction of dietary sodium, avoidance of excess fluid intake, weight reduction, and regular exercise. - A: Angiotensin II Receptor Blockers
ARBs block the effects of angiotensin II at its receptor; have similar hemodynamic effects as of ACE inhibitors. Serves as alternative for for patients who cannot tolerate ACE inhibitors. - S: Sodium restriction
A low-sodium diet (2 to 3 g/day) diet and avoidance of drinking excess amounts of fluid is recommended. - H: Hydralazine
Lowers systemic vascular resistance and left ventricular afterload.
5. Hypertension Complications "5 C's of Hypertension Complications"
The excessive pressure on the artery walls caused by hypertension or high blood pressure can damage the blood vessels, as well as organs in the body. The higher the blood pressure and the longer it goes uncontrolled, the greater the damage. With time, hypertension increases the risk of heart disease, kidney disease, and stroke.
- C: Coronary Artery Disease
Can lead to narrowing of blood vessels making them more likely to block from blood clots or fat breaking off from the lining of the blood vessel wall; also weakens the walls. - C: Chronic Renal Failure
Constant high blood pressure can damage small blood vessels in the kidneys making it not to function properly. - C: Congestive Heart Failure
Pumping blood against the higher pressure in the vessels causes the heart muscles to thicken. Eventually, the heart muscles may have a hard time pumping enough blood to meet the physiologic needs of the body leading to heart failure. - C: Cardiac Arrest
High blood pressure can cause CAD, damaged arteries cannot deliver enough oxygen to other parts of the body eventually leading to heart attack. - C: Cerebrovascular Accident
Hypertension leads to atherosclerosis and hardening of the large arteries. This, in turn, can lead to blockage of small blood vessels in the brain. It can also weaken the blood vessels in the brain causing them to balloon and burst.

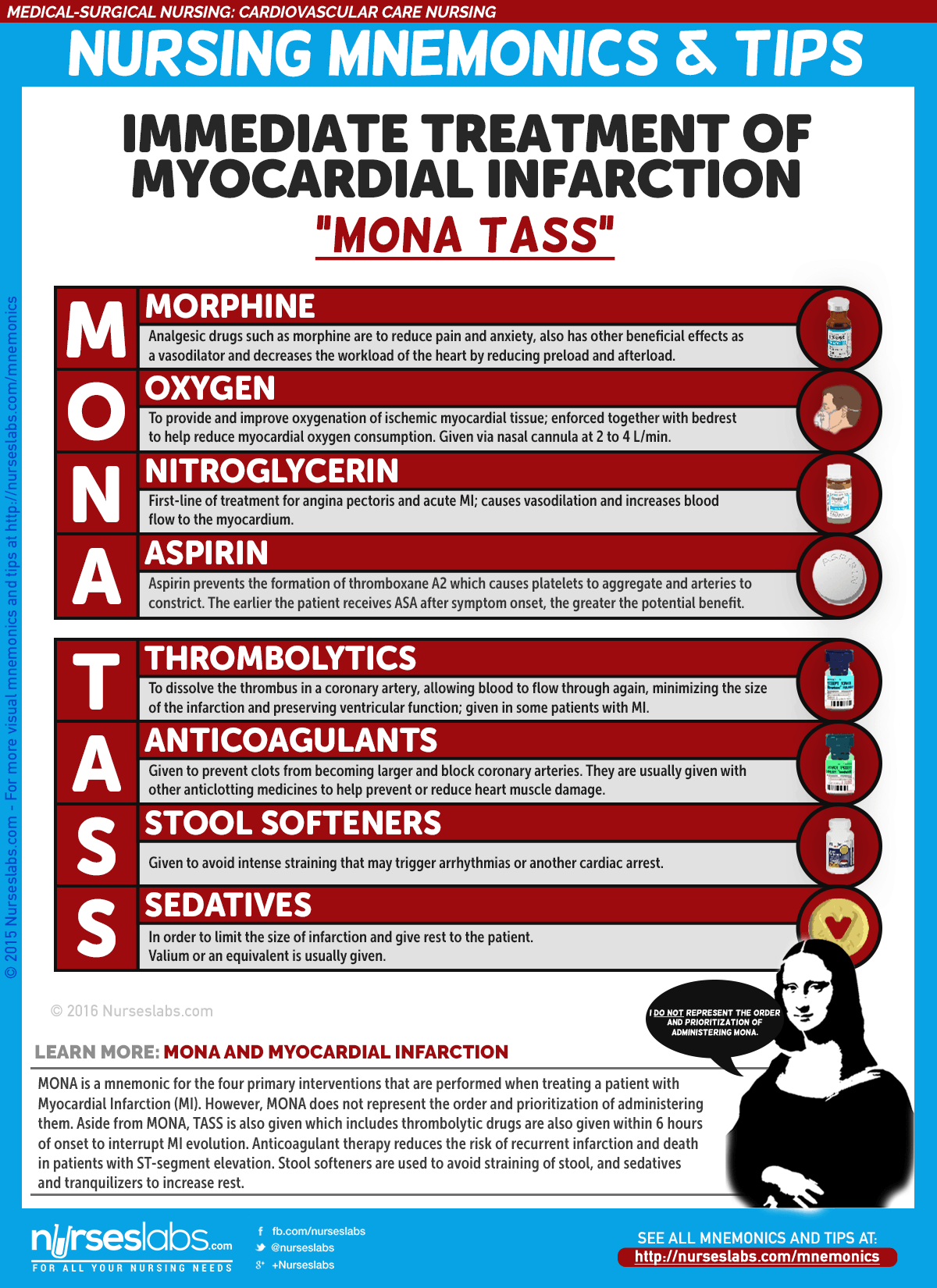
6. Immediate Treatment of a Myocardial Infarction Client "MONA TASS"
MONA is a mnemonic that stands for: Morphine, Oxygen, Nitrates, and Aspirin. These are the four primary interventions that are performed when treating a patient with Heart Attack/Myocardial Infarction (MI). However, MONA does not represent the order in which you should administer these treatments as a nurse. It is a mnemonic intended to help you remember the components of MI treatment, not the prioritization of them.
- M: Morphine
Analgesic drugs such as morphine are to reduce pain and anxiety, also has other beneficial effects as a vasodilator and decreases the workload of the heart by reducing preload and afterload. - O: Oxygen
To provide and improve oxygenation of ischemic myocardial tissue; enforced together with bedrest to help reduce myocardial oxygen consumption. Given via nasal cannula at 2 to 4 L/min. - N: Nitroglycerine
First-line of treatment for angina pectoris and acute MI; causes vasodilation and increases blood flow to the myocardium. - A: Aspirin
Aspirin prevents the formation of thromboxane A2 which causes platelets to aggregate and arteries to constrict. The earlier the patient receives ASA after symptom onset, the greater the potential benefit. - T: Thrombolytics
To dissolve the thrombus in a coronary artery, allowing blood to flow through again, minimizing the size of the infarction and preserving ventricular function; given in some patients with MI. - A: Anticoagulants
Given to prevent clots from becoming larger and block coronary arteries. They are usually given with other anticlotting medicines to help prevent or reduce heart muscle damage. - S: Stool Softeners
Given to avoid intense straining that may trigger arrhythmias or another cardiac arrest. - S: Sedatives
In order to limit the size of infarction and give rest to the patient. Valium or an equivalent is usually given.
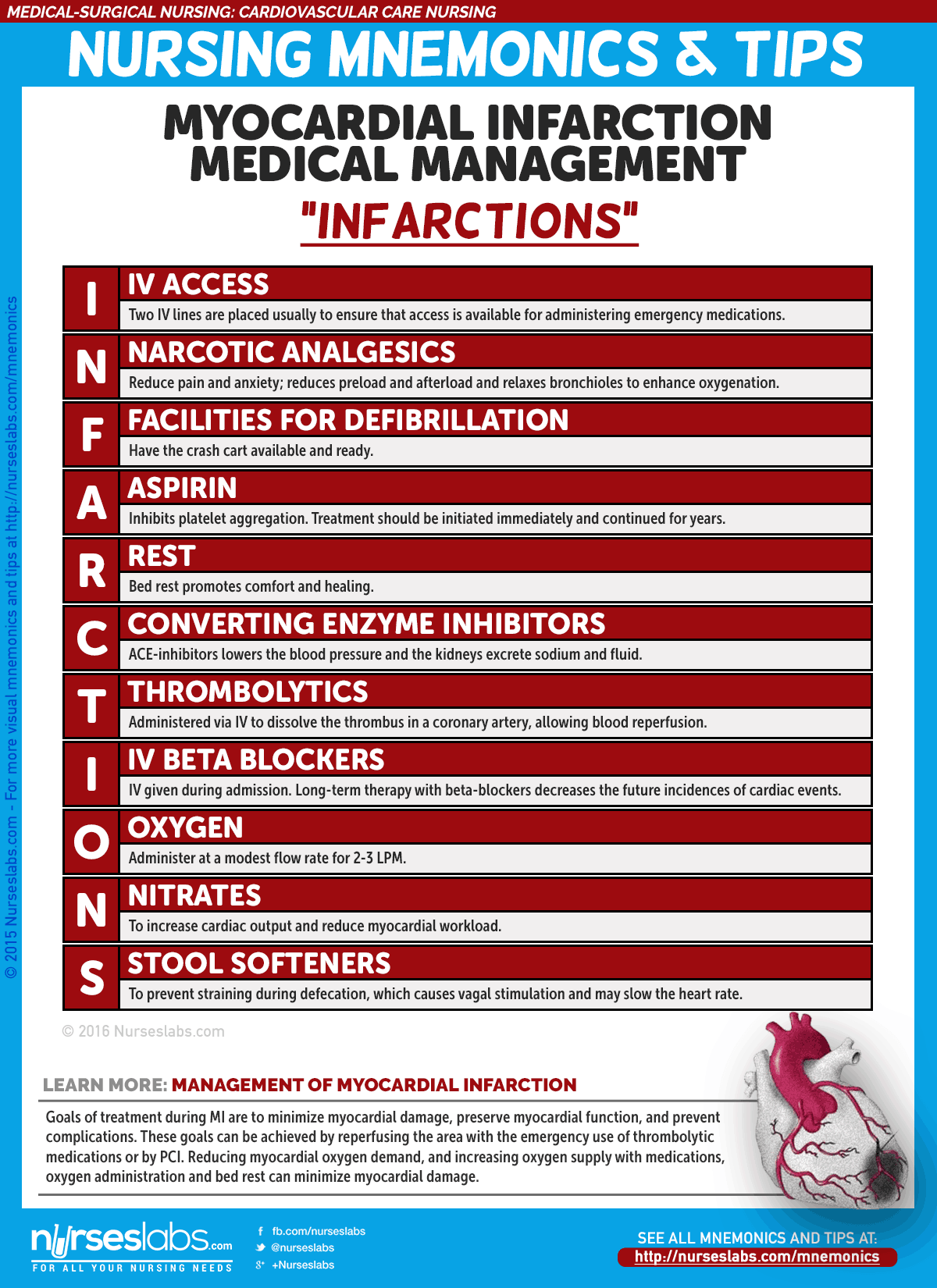
7. Myocardial Infarction Management: "INFARCTIONS"
Goals of treatment during MI are to minimize myocardial damage, preserve myocardial function, and prevent complications. These goals can be achieved by reperfusing the area with the emergency use of thrombolytic medications or by PCI. Reducing myocardial oxygen demand, and increasing oxygen supply with medications, oxygen administration and bed rest can minimize myocardial damage.
- I: IV access
Two IV lines are placed usually to ensure that access is available for administering emergency medications. - N: Narcotic analgesics
Morphine is the analgesic of choice for MI and is administered in IV boluses to reduce pain and anxiety; reduces preload and afterload and relaxes bronchioles to enhance oxygenation. - F: Facilities for defibrillation (DF)
Have the crash cart available and ready. - A: Aspirin
Inhibits platelet aggregation. Treatment should be initiated immediately and continued for years. - R: Rest
Bed rest promotes comfort and healing. - C: Converting enzyme inhibitor
ACE-inhibitors lowers the blood pressure and the kidneys excrete sodium and fluid. - T: Thrombolytics
Administered via IV to dissolve the thrombus in a coronary artery, allowing blood reperfusion, minimizing the size of the infarction and preserving ventricular function. - I: IV beta blocker
Long-term therapy with beta-blockers decreases the future incidences of cardiac events. - O: Oxygen
Administer at a modest flow rate for 2 to 3 LPM. - N: Nitrates
To increase cardiac output and reduce myocardial workload; relieves pain by redistributing blood to ischemic areas of the myocardium. - S: Stool Softeners
To prevent straining during defecation, which causes vagal stimulation and may slow the heart rate.
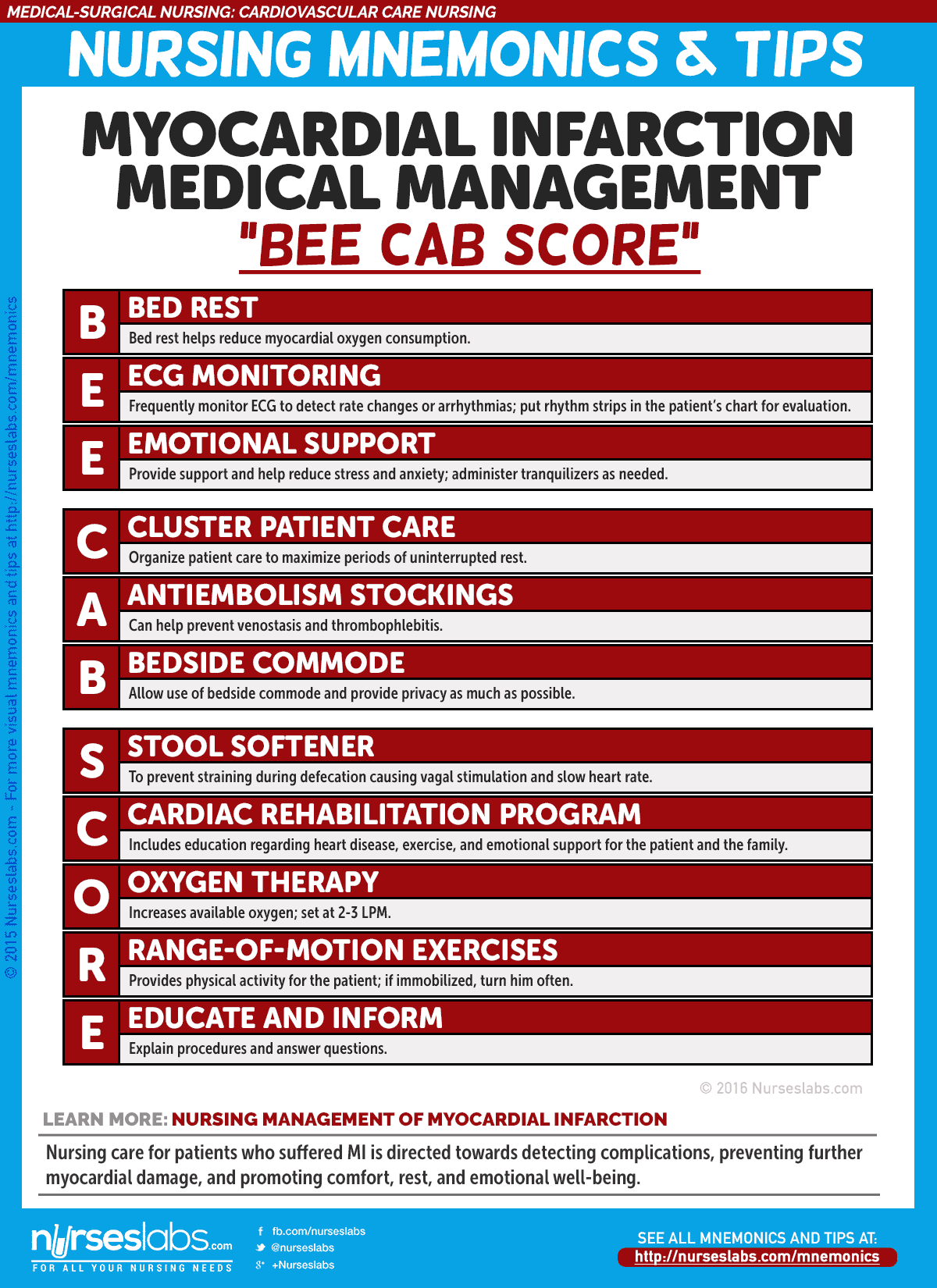
8. Myocardial Infarction Nursing Management: "BEE CAB SCORE"
Nursing care for patients who suffered MI is directed towards detecting complications, preventing further myocardial damage, and promoting comfort, rest, and emotional well-being.
- B: Bed rest
Bed rest helps reduce myocardial oxygen consumption. - E: ECG Monitoring
Frequently monitor ECG to detect rate changes or arrhythmias; place rhythm strips in the patient's chart for evaluation. - E: Emotional support
Provide support and help reduce stress and anxiety; administer tranquilizers as needed. - C: Cluster/Organize Patient Care
To maximize periods of uninterrupted rest. - A: Antiembolism stockings
Can help prevent venostasis and thrombophlebitis. - B: Bedside commode
Allow use of bedside commode and provide privacy as much as possible. - S: Stool Softener
To prevent straining during defecation causing vagal stimulation and slow heart rate. - C: Cardiac Rehabilitation Program
Includes education regarding heart disease, exercise, and emotional support for the patient and the family. - O: Oxygen therapy
Increases available oxygen; set at 2-3 LPM. - R: Range-of-motion Exercises
Provides physical activity for the patient; if immobilized, turn him often. - E: Educate and inform
Explain procedures and answer questions.
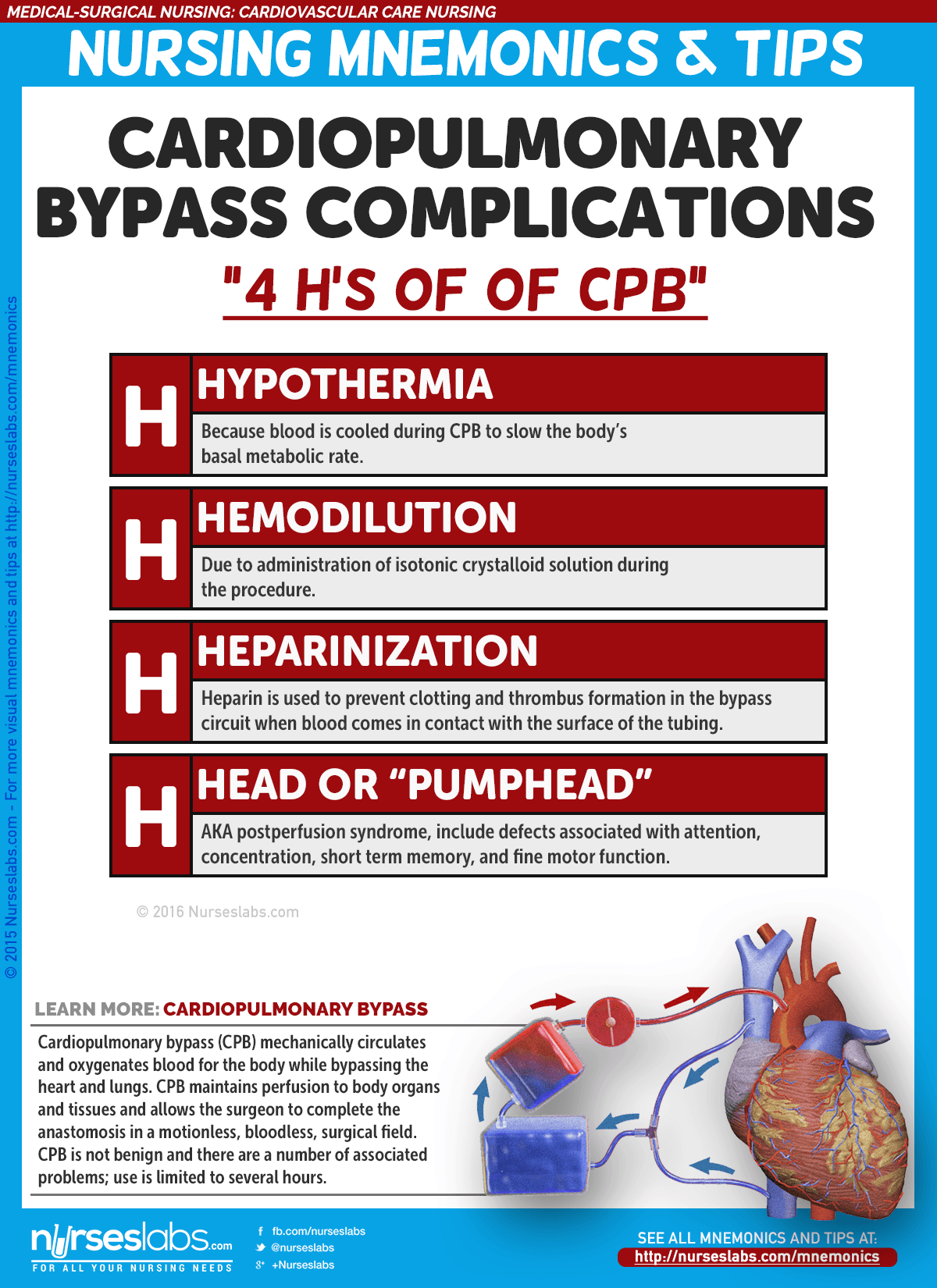
9. Cardiopulmonary Bypass Complications "4 H's of CBP"
Cardiopulmonary bypass (CPB) mechanically circulates and oxygenates blood for the body while bypassing the heart and lungs. CPB maintains perfusion to body organs and tissues and allows the surgeon to complete the anastomosis in a motionless, bloodless, surgical field. CPB is not benign and there are a number of associated problems; use is limited to several hours.
- H: Hypothermia
Because blood is cooled during CPB to slow the body's basal metabolic rate. - H: Hemodilution
Due to administration of isotonic crystalloid solution during the procedure. - H: Heparinization
Heparin is used to prevent clotting and thrombus formation in the bypass circuit when blood comes in contact with the surface of the tubing. - H: Head or "Pumphead"
AKA postperfusion syndrome, include defects associated with attention, concentration, short term memory, fine motor function, and speed of mental and motor responses.
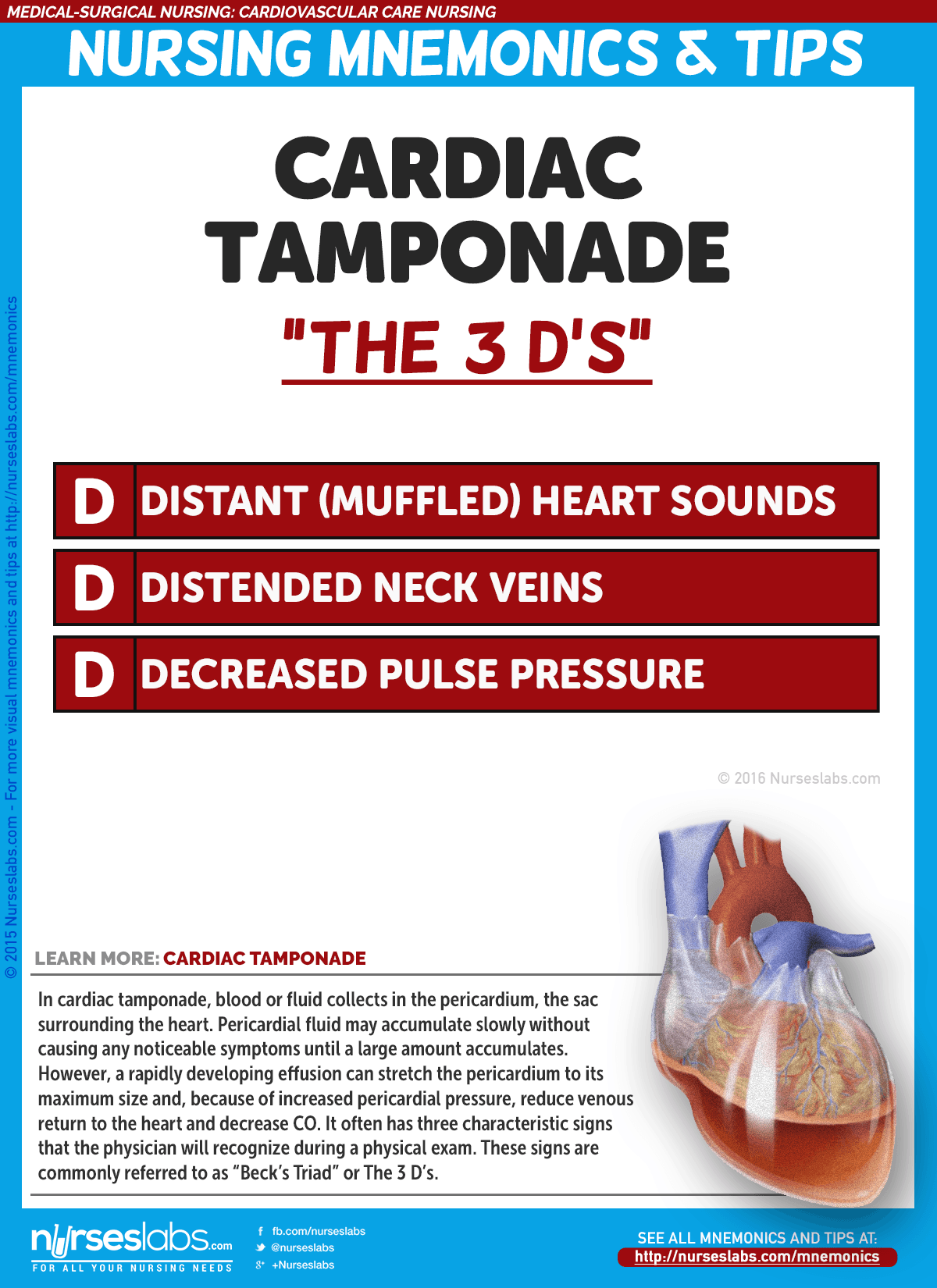
10. The "3 D's" Cardiac Tamponade (Beck's Triad)
In cardiac tamponade, blood or fluid collects in the pericardium, the sac surrounding the heart. Pericardial fluid may accumulate slowly without causing any noticeable symptoms until a large amount accumulates. However, a rapidly developing effusion can stretch the pericardium to its maximum size and, because of increased pericardial pressure, reduce venous return to the heart and decrease CO. It often has three characteristic signs that the physician will recognize during a physical exam. These signs are commonly referred to as "Beck's Triad" or The 3 D's.
- D: Distant or muffled heart sounds
- D: Distended jugular veins
- D: Decreased pulse pressure
More to be added soon…
Know a few witty nursing mnemonics? If you some mnemonics about this topic, please do share them at our comments section below! Also, there are more nursing mnemonics here, be sure to check them out.
Source: https://nurseslabs.com/cardiovascular-care-nursing-mnemonics-tips/
0 Response to "Easy to Remember Asthma Fnp Study Guide"
Postar um comentário